UK Domestic TB Update 2025
Read below to learn about the latest updates on tuberculosis in the UK as of 2025.
This work was collated by Marc Lipman (Clinical Lead, UKAPTB) with the support of Sharon Cox, Suzi Coles, Jeff Featherstone, Steve Hindle, Adele Mackin and Ezabella Ayele.
Case Reports
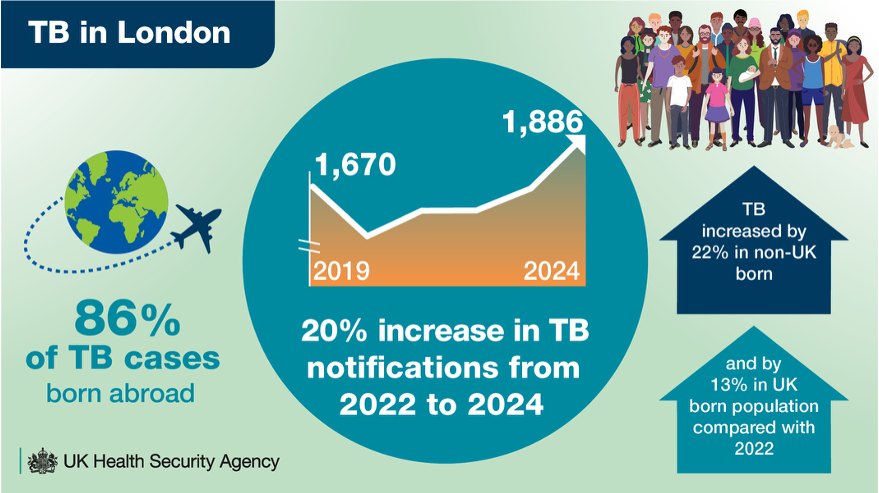
Between 2022 and 2024 the UK Health Security Agency has reported a 25% increase in Tuberculosis (TB) cases across England with increases seen in many individual regions, such as Yorkshire and Humber, the North East, London and the East Midlands.
Alongside an increase in overall reported TB cases there is an increasing number of Drug Resistant TB (DR-TB), Multi Drug Resistant TB (MDR-TB) cases and Extremely Drug Resistant TB (XDR-TB) cases.
DR-TB, MDR-TB and XDR-TB patients face worse outcomes and longer treatments.
In these patients, the bacteria which cause the deadly disease (TB) are resistant to drugs that are designed to target them.
Read more about MDR-TB here (WHO, Results UK, LSTM)
Ongoing Treatment Shortages
There is an ongoing shortage of treatments for TB (also called drug stockouts) globally and in the UK. These ongoing shortages are putting patient care, public health and TB control efforts at risk. Here’s why this is a serious problem:
Impact on Patient Care
People receive less effective treatment
Drug shortages mean some patients can't get the most effective medications. This leads to sub-optimal care and reduces their chances of full recovery.
Treatment is interrupted or delayed
TB treatment needs to be taken consistently over many months. When medicines run out, treatment plans are disrupted, which puts patients health at risk.
Patients have to take more tablets
Fixed-dose combination (FDC) pills combine multiple drugs into one tablet. When these aren’t available, patients must take more tablets each day, making it harder to stick to treatment.
More chance of mistakes and side effects
Complex or unfamiliar drug regimens increase the risk of prescribing errors, side effects, and patients stopping treatment early.
Barriers to Newer, More Effective Treatment
Newer, shorter treatments are unavailable
Important drugs like Rifapentine and Pretomanid, which have shorter TB treatment plans, are not available in the UK. This is despite the fact that these treatment plans and drugs are approved and used in other countries.UK patients treatment could fall behind global standards
The UK cannot currently offer the most up-to-date, WHO-recommended treatments, which is leaving patients with longer, more difficult, and less effective options.
Wider Public Health Risks
Drug-resistant TB can become more prevalent
Incomplete or irregular treatment increases the risk that bacteria that cause TB become resistant to drugs, which can make future cases harder to treat.TB spreads more easily
When people with TB aren’t treated quickly and effectively, they stay infectious for longer. This can increase the risk of passing TB on to other people.Opportunities to prevent TB are missed
Shortages affect not just those with active TB, but also people who need preventive treatment for latent TB (a form of TB where the bacteria is not currently causing disease but will in the future if not treated). Delays can mean more future TB cases.
Systemic and Cost Implications
Frontline services are caught off guard
NHS providers often get no advance warning of stockouts, making it difficult for healthcare providers to plan or protect patients during shortages.Public investment isn’t improving access
Despite significant public funding used to develop life-saving TB drugs (like Bedaquiline), prices remain high and access is limited, even within the NHS.The most vulnerable are affected the most
People already facing barriers to care, due to housing, income, or immigration status, are disproportionately affected by these drug shortages.
So what do we need to tackle stockouts:
A stronger, more reliable TB drug supply chain
Early warning systems for stockouts to help NHS services plan ahead
Better access to newer, more effective TB medicines
Fair pricing and contracts to ensure affordability and availability
Government leadership to bring UK TB care up to international standards
Groups and Action Plans
TB Task and Finish Group 2024
The UK Health Security Agency (UKHSA) was tasked by the Chief Medical Officer (CMO) and Medical Director of NHS England to develop policy options focused on prevention and improving access to care for TB. This involved:
A Cross-Government Initiative: A collaborative effort involving the Home Office, Foreign Commonwealth and Development Office (FCDO), Department of Health and Social Care (DHSC), NHS England, and UKHSA.
Working Groups Established (April 2025): Multidisciplinary groups launched with clinical, nursing, and health protection experts to explore policy options and strengthen testing and treatment for latent TB infection (LTBI).
Patient & Public Involvement: Led by UKHSA’s Health Equity team to ensure inclusive and representative input.
Expert Advisory Structures: A Clinical and Academic Reference Group has been convened to provide evidence-based guidance.
Progress Update: An interim report has been reviewed by UKHSA’s Chief Medical Advisor and is now under consideration by the CMO and Co-National Medical Director.
TB Action Plan 2021-2026
Current Strategy (2021–2026): The TB Action Plan aims to improve the prevention, detection, and control of TB in England.
Planning for Post-2026: Work is already underway across UKHSA, DHSC, and NHS England to plan the future TB strategy, focusing on:
Scope: Defining the vision and priorities for TB control beyond 2026.
Governance: Establishing clear leadership and accountability structures.
Resources: Identifying the funding and capacity needed to deliver long-term impact.
Co-Production at the Core: The future TB strategy will be developed through meaningful involvement from patients, communities, researchers and healthcare professionals.
Call for Evidence to inform the TB Action Plan 2026
The UKHSA launched a call for evidence via their website, lasting for a month in April 2025, inviting input to inform the 2026–2031 TB National Action Plan.
The call welcomed contributions from the public, stakeholders, technical experts, and individuals with lived experience of TB.
From the 193 responses received, the major themes identified were the need for:
Improved diagnostic capabilities and access to appropriate medications.
Investment in workforce development and service delivery models.
A deeper understanding of the impact of population risk factors and social determinants of health on TB control
Next Steps include a full analysis of the responses, to be published in Autumn 2026, providing valuable insights to guide the national strategy.
Getting It Right First Time (GIRFT) TB Programme
Royal National Orthopaedic Hospital
What is the GIRFT TB programme?
The Getting It Right First Time (GIRFT) TB Programme is an initiative commissioned by NHS England, which is designed to support high-quality, efficient, and consistent care for people affected by TB in England.
The programme objectives are to:
Identify care processes and opportunities for improvement
Reduce delays in diagnosis and treatment for patients
Understand the current TB workforce to inform future planning
Provide support for:
Service transformation
The Latent TB programme
Implementation of the National TB Action Plan
The programme does not include Children and young people (CYP), Non-tuberculous mycobacteria (NTM) and TB diagnostics.
The final output was a report including:
Evidence-based recommendations
Examples of good practice.
What did GIRFT TB find?
Survey Engagement:
120 surveys distributed
117 responses received, which demonstrates strong engagement from TB services.
Service-Level Reporting:
A tailored data pack was produced for each TB service, which included:
286 slides per service
A core slide deck
This data back was shared with TB service providers and Integrated Care Boards (ICBs)
Key Findings:
As anticipated, the data revealed unwarranted variation in care across regions
Extensive examples of excellent practice were identified and can inform recommendations.
GIRFT Review of Tuberculosis, National Report: England
Summary:
79 pages covering a wide range of topics and challenges
81 recommendations given
Good practice guides for care
The report has been signed off by NHS England.
Areas the report covers:
1. Responsibilities, Policy & Payment
National, regional, and ICB-level TB policies
Services for underserved populations
Notification of TB surveillance (NTBS) and data capture quality
Payment mechanisms and clinical coding
Education and training provision
Integration with ongoing and future research priorities
2. Clinical Care
Diagnosis of TB and pathways to care
Inpatient and outpatient management
Medicines management and treatment adherence
Treatment adherence including the use of:
Directly Observed Therapy (DOT)
Video Observed Therapy (VOT)
Challenges outstanding or not scoped in:
Non-tuberculous mycobacteria (NTM)
Multidrug-resistant (MDR/XDR) TB
Children and young people (CYP)
3. Workforce
A mapping of capacity and configuration of the:
Medical workforce
Nursing staff
Administration support.
4. Prevention
BCG vaccination programmes
Contact tracing effectiveness and follow-up
Latent TB infection (LTBI): service delivery and preventive treatment.
GIRFT TB implementation framework
NHS England commissioned RNOH / GIRFT TB Programme Team to support implementation of these recommendations.
The Aims of the implementation framework were to:
Ensure that all key stakeholders are aware of the report and findings
Ensure all parties work towards implementation of recommendations
Ensure all stakeholders are appraised of progress
Ensure that good practice examples are shared
Highlight any areas of risk during implementation and attempt mitigation.
In order to successfully deliver the implementation framework the group:
Publicised the report and recommendations
Set up an Implementation Oversight Group
Met with individual Regions
Meeting with ICBs and providers
GIRFT TB progress to date and future work
The implementation of the GIRFT TB Programme recommendations is underway, with significant engagement and coordination across the system.
Progress to Date:
National webinar held to launch the implementation, accompanied by a toolkit issued to all services
Meetings with all Regional Medical Directors and Regional Chief Nurses
Engagement with ICBs and TB service providers (8 meetings held in total)
Bi-monthly Implementation Oversight Group (IOG) meetings, with early engagement on education and medicines management underway.
Next Steps:
Stakeholder meetings to be scheduled with UKHSA, NHS England, and others
Second round of regional meetings, planned for September-October 2025
Webinar or face-to-face event to share good practice, planned for February 2026
Conclusions and final Implementation Report to be published in March 2026.
GIRFT TB - Risks and Challenges
Progress is being made through GIRFT TB, but several challenges have been identified requiring monitoring throughout implementation:
Lack of TB Leads in Regions and systems
TB leads are not always identified or designated which can hinder progress. Regions are now identifying TB leads and confirming names.
Work is ongoing to identify and confirm ICB TB leads.
Lack of awareness of the National Report:
Awareness of the GIRFT TB report remains limited in some NHS England regions and local systems, which may hinder engagement.
Varied response to the recommendations in systems & services:
This is being addressed through targeted process meetings.
Organisational changes at NHS England/Regions/Systems:
Structural changes within NHS England, regions, and local systems can impact ownership and continuity of implementation efforts.
Uncertainties around implementing the 10-year plan.
Lack of available funding to support change.
TB in the 10 Year Health Plan: England
Tuberculosis is highlighted in the 10 Year NHS Health Plan as an example of a high-impact antimicrobial resistant infection, with significant human and financial costs to the health system.
Key areas within the plan include:
Prevention-Focused Care
Latent TB infection (LTBI) testing and treatment readily fits within the shift from treating illness to preventing it, reaching patients earlier, reducing transmission and improving outcomes.Neighbourhood Health Service Model:
This model supports accessible and continuous care for TB in local communities. This includes prioritising LTBI testing being integrated into local care services where appropriate.Technology and Data for Detection:
Emphasis on early detection of infectious diseases through improved technology and data use. Better data is also critical to support prevention and address health inequalities.
Call for Coordinated Action:
Successful implementation of TB services requires ongoing focus at both national and local levels to keep TB on the agenda.
Future Delivery Models and NHS System Changes
NHS England is working closely with UKHSA to explore future delivery models for TB care as part of the development of the new TB Action Plan.
They are also:
Adapting to Systemic Changes:
The reconfiguration of Integrated Care Boards (ICBs) offers an opportunity to review and refine targeting in a nationally funded programme, taking into account the current migration patterns.Ongoing Programme Delivery:
NHS England is continuing to work with providers, commissioners, and regional colleagues to deliver the existing TB programme.Supporting Implementation:
NHS England is working with GIRFT and partners to support the implementation of GIRFT TB recommendations.